How Do We Understand Asthma Better From Ct Imaging
Computed tomography has provided mainly structural information on the lungs and airways in asthma, while other expiratory CT studies have provided functional data on small airways function that have confirmed their importance in pathophysiology. Whole-body CT scans provide imaging down to the small conducting airways . The ability to see airways clearly is based on the contrast difference between airway and soft tissue, and, unsurprisingly, the accuracy of airway measurements decreases with decreasing airway size .
CT image resolution is most limited in the z-direction, i.e. longitudinal axis. Modern high-resolution scans often use the helical or spiral mode . During helical or spiral mode scanning, the X-ray tube rotates while the patient is moved through the tube, hence any single image capture element effectively makes a helical motion along the chest wall. The advantage is speed, which allows imaging the entire lung in one hit and during a single breath-hold. Hence, the anatomical localisation of all structures in the chest, in the resultant three-dimensional image is accurate . The disadvantage is loss of information: reduced resolution, depending on how fast the subject is moved through the scanner .
Understanding Asthma From Functional Ct Imaging Studies
Changes in ventilation distribution are a fundamental characteristic of many lung diseases, including asthma. Ventilation distribution measured using complex lung function tests, such as inert gas washout, has been shown to be highly heterogeneous that is, some parts of the lung function well, while other parts function poorly, making ventilation highly variable within a lung. This concept is referred to as ventilation heterogeneity or ventilation inhomogeneity and has been shown to be strongly correlated with airway hyperresponsiveness , asthma symptoms , medication requirements and asthma severity . Ventilation imaging complements these lung function tests of ventilation distribution, by providing information on three-dimensional location and organisation. However, much of the clinical and physiological significance of parameters that quantify three-dimensional ventilation still needs to be determined.
a, b) Inspiratory and c, d) expiratory computed tomography scans from the same subject, at two levels. The image in a) is at approximately the same anatomical location as c) and b) is at approximately the same location as d). The arrows on the expiratory images indicate regions of gas trapping due to severe narrowing and airway closure.
Microbes And The Host
A key feature of any microorganism is its ability to be recognised and sampled by the immune system. The ensuing immune response, depending on the microbe, can range from benign tolerance to acute inflammation and injury, with ensuing repair and remodelling in the lungs . Respiratory fungi, bacteria and viruses are recognised by innate receptors including Toll-like receptors , RIG-1-like helicases and NOD-like receptors which when stimulated then activate the nuclear factor B group transcription factors with the possible resultant induction of more than 100 pro-inflammatory and host response genes . Microorganisms can affect the permeability of the epithelium increasing infection risk, affecting epithelial integrity by invasion of the epithelium cells leading to cell death and shedding. By compromising the epithelium, subsequent allergen uptake and the effect of environmental exposure to pollutants may cause an increased possibility for the development of further exacerbations and a heightened immune response increasing the risk of a pathogenic response and asthma development .
It is believed that microaspiration, which occurs in healthy individuals but has a higher prevalence in asthmatics, could in part explain the presence of oral microbiota in the lower lung . However this does not fully explain why some individuals have a higher relative abundance of certain bacteria originating from the upper respiratory tract .
You May Like: Medications Used To Treat Asthma
Learn More About Asthma
A general public education video created by the American Lung Association for use with patients in schools and clinics. This 3-minute video simplifies how lungs work and shows how lungs are an essential part of the respiratory system.
This booklet offers the latest information on asthma management. In an easy-to-read format, it provides information about asthma symptoms, the latest treatments, and ways to monitor and keep your asthma under control. This site also includes the Clinical Guidelines for the Diagnosis and Management of Asthma and What Is Asthma?
The Asthma Basics course is a free, one-hour interactive online learning module designed to help people learn more about asthma. This course is ideal for frontline healthcare professionals like nurses or community health care workers, as well as individuals who have asthma. Asthma Basics also includes comprehensive resources like asthma medication devices, and demonstration videos and downloads. This course is also available in Spanish.
What Asthma Treatment Options Are There

You have options to help manage your asthma. Your healthcare provider may prescribe medications to control symptoms. These include:
- Bronchodilators: These medicines relax the muscles around your airways. The relaxed muscles let the airways move air. They also let mucus move more easily through the airways. These medicines relieve your symptoms when they happen and are used for intermittent and chronic asthma.
- Anti-inflammatory medicines: These medicines reduce swelling and mucus production in your airways. They make it easier for air to enter and exit your lungs. Your healthcare provider may prescribe them to take every day to control or prevent your symptoms of chronic asthma.
- Biologic therapies for asthma: These are used for severe asthma when symptoms persist despite proper inhaler therapy.
You can take asthma medicines in several different ways. You may breathe in the medicines using a metered-dose inhaler, nebulizer or another type of asthma inhaler. Your healthcare provider may prescribe oral medications that you swallow.
Recommended Reading: Does Elderberry Help With Asthma
What Is The Pathophysiology Of Asthma
To understand the pathophysiology of asthma, we first need to understand what exactly is the pathophysiology? Also, why is it necessary to write one?
To explain pathophysiology in layman language, it combines physiology with pathology. The study of a disorder or injury, its causes, effects and diagnosis are called pathophysiology. Pathology is concerned with the physical changes and effects a disease has on the patient. In contrast, physiology studies the biological and internal changes in the patients condition.
Dupilumab, a biotech drug, helps reduce asthma attacks and increase lung function, research shows.
Some of you might wonder, Why is it important to write a pathophysiology paper?
Such informative writing is an essential part of a medicine and nursing curriculum, and all nursing students must write one. Nurses are responsible for creating and monitoring the case data for various patients in the hospital. A pathophysiology paper provides all the necessary information regarding the condition, effects and development in a patients condition that are necessary for the doctors to treat the patient.
Key Differences From 1997 And 2002 Expert Panel Reports
- The critical role of inflammation has been further substantiated, but evidence is emerging for considerable variability in the pattern of inflammation, thus indicating phenotypic differences that may influence treatment responses.
- Gene-by-environmental interactions are important to the development and expression of asthma. Of the environmental factors, allergic reactions remain important. Evidence also suggests a key and expanding role for viral respiratory infections in these processes.
- The onset of asthma for most patients begins early in life with the pattern of disease persistence determined by early, recognizable risk factors including atopic disease, recurrent wheezing, and a parental history of asthma.
- Current asthma treatment with anti-inflammatory therapy does not appear to prevent progression of the underlying disease severity.
Asthma is a common chronic disorder of the airways that involves a complex interaction of airflow obstruction, bronchial hyperresponsiveness and an underlying inflammation. This interaction can be highly variable among patients and within patients over time. This section presents a definition of asthma, a description of the processes on which that definition is basedthe pathophysiology and pathogenesis of asthma, and the natural history of asthma.
You May Like: What Helps Asthma When No Inhaler
Additional References For Asthma
Control Of Triggering Factors
Triggering factors in some patients may be controlled with use of synthetic fiber pillows and impermeable mattress covers and frequent washing of bed sheets, pillowcases, and blankets in hot water. Ideally, upholstered furniture, soft toys, carpets, curtains, and pets should be removed, at least from the bedroom, to reduce dust mites and animal dander. Dehumidifiers should be used in basements and in other poorly aerated, damp rooms to reduce mold. Steam treatment of homes diminishes dust mite allergens. House cleaning and extermination to eliminate cockroach exposure are especially important. Although control of triggering factors is more difficult in urban environments, the importance of these measures is not diminished.
High-efficiency particulate air vacuums and filters may relieve symptoms, but no beneficial effects on pulmonary function and on the need for drugs have been observed.
Sulfite-sensitive patients should avoid sulfite-containing food .
Patients with aspirin-sensitive asthma can use acetaminophen, choline magnesium salicylate, or highly selective NSAIDs like celecoxib when they need a pain reliever.
Asthma is a relative contraindication to the use of nonselective beta-blockers , including topical formulations, but cardioselective drugs probably have no adverse effects.
Also Check: First Line Of Treatment For Asthma
Pathophysiology And Pathogenesis Of Asthma
Airflow limitation in asthma is recurrent and caused by a variety of changes in the airway. These include:
CYTOKINE BALANCE Numerous factors, including alterations in the number or type of infections early in life, the widespread use of antibiotics, adoption of the Western lifestyle, and repeated exposure to allergens, may affect the balance between Th1-type
There also appears to be a reciprocal interaction between the two subpopulations in which Th1 cytokines can inhibit Th2 generation and vice versa. Allergic inflammation may be the result of an excessive expression of Th2 cytokines. Alternatively, recent studies have suggested the possibility that the loss of normal immune balance arises from a cytokine dysregulation in which Th1 activity in asthma is diminished. The focus on actions of cytokines and chemokines to regulate and activate the inflammatory profile in asthma has provided ongoing and new insight into the pattern of airway injury that may lead to new therapeutic targets.
Genetics
Sex
In early life, the prevalence of asthma is higher in boys. At puberty, however, the sex ratio shifts, and asthma appears predominantly in women . How specifically sex and sex hormones, or related hormone generation, are linked to asthma has not been established, but they may contribute to the onset and persistence of the disease.
Environmental Factors
Allergens
Respiratory infections
Other environmental exposures
Environmental Remediation For Asthma
The medical management of asthma and treatment of acute attacks has improved substantially, but the prevalence of asthma continues to rise in urban settings in industrialized Western countries. There is still controversy about the hygiene hypothesis, and it is not yet clear that early exposure to certain antigens could be exploited as a preventive measure. Given what is known about asthma, avoidance of asthma trigger factors would be expected to at least reduce the frequency and severity of symptoms. EPA recommendations for an “Asthma Friendly House” are shown in the iFrame below.
EPA Recommendations Asthma Friendly House
For additional measures, also see the EPA Home Environment Checklist.
There is some evidence that interventions to reduce dust, animal dander, mold, and exposure to cockroaches are effective, but the literature indicates that allergen reduction is difficult to achieve and the effectiveness is not as great as expected. The four articles cited below suggest that environmental remediation interventions that target one or two potential targets are of limited, if any value. However, they suggest that multifaceted interventions can reduce symptoms, school absences, and hospital visits for acute asthma care.
From the Abstract:
Results
Summary:
From the Abstract:
“Evidence synthesis
Summary
Read Also: Can Asthma Cause Shortness Of Breath Without Wheezing
The Mycobiome And Asthma
It has been reported by Black et al., in 37 patients admitted to the ICU for an acute asthma attack, that 54% tested positive in a skin test for fungal spores which included Alternaria tenuis, Cladosporium cladosporides, Epicoccum nigrum and Helminthosporium maydis . O Driscoll et al., recruited 181 patients, aged between 16 and 60 years of age and divided them into three groups severe, moderate and mild, dependent on their number of lifetime hospital admissions. 76% of patients with severe asthma tested positive in a skin test toone or more moulds including Aspergillus fumigatus, Penicillium notatum, Cladosporium herbarum, Alternaria alternata or the yeast Candida albicans in comparison to lower rates of positivity in patients with moderate or mild asthma .
Exposure to fungal allergens can have a devastating impact onasthmatics. Fungi contain proteins which are detrimental to the airway epithelium, enhance additional reactions and also act as allergens . It is possible that the long term fungal colonisation of an atopic patient may provide a chronic source of allergen exposure, propagate airway inflammation and increase severity of asthma phenotype .
Asthma Pathophysiology Diagnosis Medical Management & Nursing Care
Asthma pathophysiology involves chronic inflammation of the airways that causes bronchoconstriction , leading to airway hyperresponsiveness , excessive mucus production and retention , and airway oedema. Asthmatic patients with airway inflammation, which is reversible, tend to experience symptom-free periods as well as acute asthma exacerbations.
Causes of asthma include allergies, exposure to airway allergens and air pollutants, exercise, stress, and medication such as NSAIDS and non-selective Type 2 Beta Blockers.
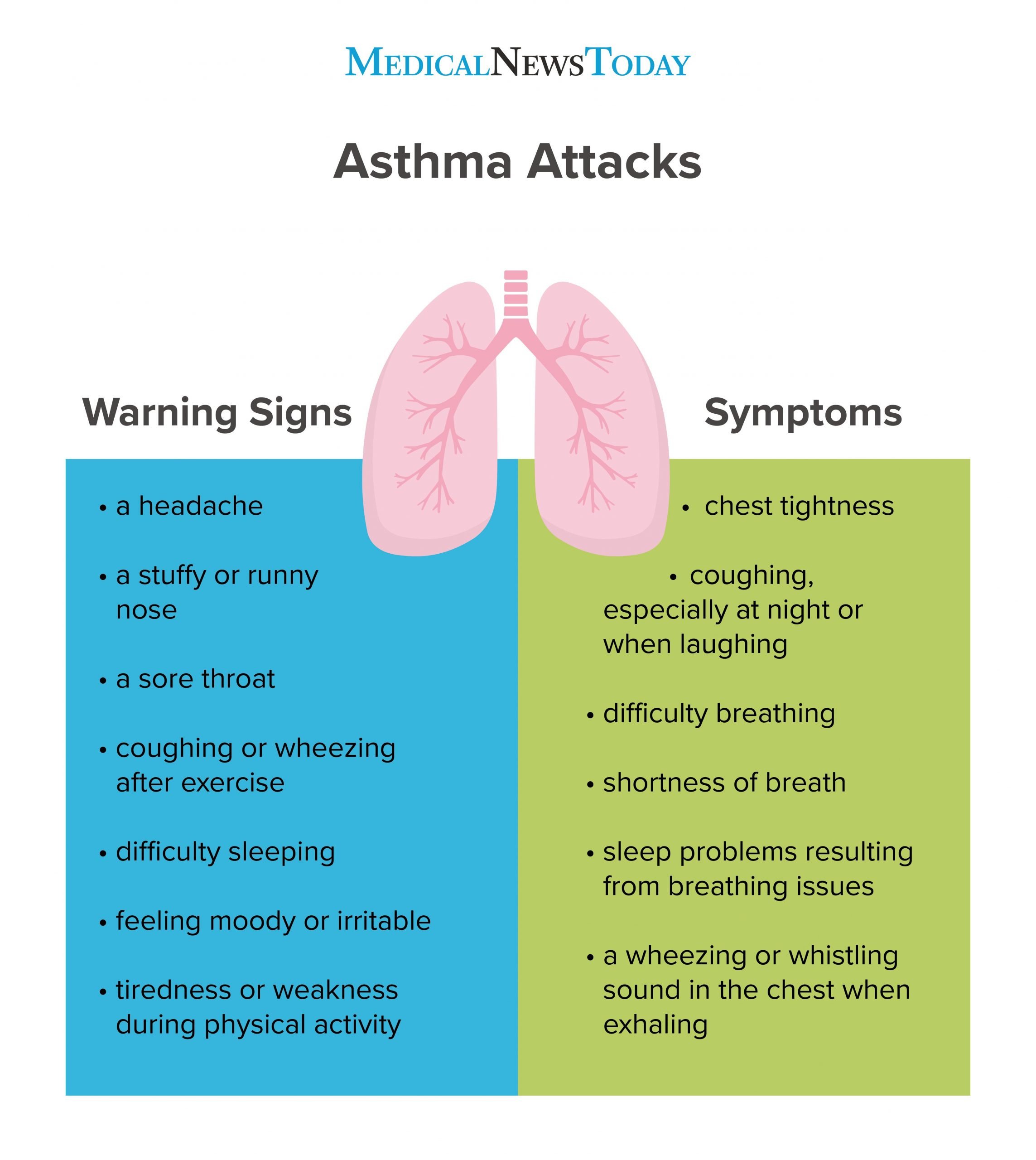
Asthma Signs and Symptoms:
- Widened pulse pressure
- Other comorbidities such as GERD, COPD or respiratory tract infections increase risk for asthma
Asthma Complications:
- Status asthmaticus
- Respiratory failure
Asthma Diagnosis Factors:
- Peak Expiratory Flow Rate
- Respiratory acidosis is a very common acid base disturbance in acute severe asthma. Its early recognition and treatment is vital for the final outcome, as it can lead to respiratory failure and arrest if prolonged.
Asthma Pharmacological Therapy
QUICK RELIEF
LONG TERM MEDICATION
- inhaled corticosteroids eg. Budesonide administered as prophylaxis of acute asthma exacerbation
- long-acting beta 2 adrenergic agonists eg. Tiotropium
- Methylxanthines eg. Theophylline
Additional Interventions
Monitoring an Asthmatic Patient Post-Treatment
Below you can find a collection of videos that can help provide a more visual approach to asthma pathophysiology, diagnosis, medical management and nursing care.
Also Check: What Is The Best Treatment For Allergic Asthma
Pathophysiology Of Asthma: Causes And Diagnosis
Asthma is a long persisting breathing condition the patient’s breathing tract inflates due to varied reasons, which causes difficulty in breathing. There isn’t a sole defined cause of asthma it is caused due to many factors like microparticles in the environment, genetic factors, allergies, and tobacco smoking.
Even though over 5.4 million individuals in the UK have asthma, no certified test is available, and the diagnosis is solely suggested based on symptoms.
Pathophysiology of asthma will help you understand the patient’s condition in detail and suggest an effective diagnosis. The origin of asthma has changed in the last 25 years, as researchers have discovered multiple asthma compositions.
Various pathological factors are involved with asthma, such as airway blockage due to inflamed bronchi and coughing, difficulty breathing, and wheezing. Asthma affects the various parts of the airway, trachea, bronchi, and bronchioles. Inflammation persists even when breathing difficulty isn’t obvious.
Why Is My Asthma Worse At Night
Asthma that gets worse at night is sometimes called nighttime asthma or nocturnal asthma. There are no definite reasons that this happens, but there are some educated guesses. These include:
- The way you sleep: Sleeping on your back can result in mucus dripping into your throat or acid reflux coming back up from your stomach. Also, sleeping on your back puts pressure on your chest and lungs, which makes breathing more difficult. However, lying face down or on your side can put pressure on your lungs.
- Triggers in your bedroom and triggers that happen in the evening: You may find your blankets, sheets and pillows have dust mites, mold or pet hair on them. If youve been outside in the early evening, you may have brought pollen in with you.
- Medication side effects: Some drugs that treat asthma, such as steroids and montelukast, can affect your sleep.
- Air thats too hot or too cold: Hot air can cause airways to narrow when you breathe in. Cold air is an asthma trigger for some people.
- Lung function changes: Lung function lessens at night as a natural process.
- Asthma is poorly controlled during the day: Symptoms that arent controlled during the day wont be better at night. Its important to work with your provider to make sure your asthma symptoms are controlled both day and night. Treating nighttime symptoms is very important. Serious asthma attacks, and sometimes deaths, can happen at night.
Also Check: What Kind Of Doctor Do You See For Asthma
Allergy And The Immune System
Many researchers have tried to identify the main causes of airways inflammation. Abnormalities of the immune system, which protects our bodies from infection, have been thought to be major contributors to the development of asthma. More specifically, allergic responses have been considered to be the main determinants of the asthma phenotype. Extensive research over the years, however, has shown that there are different phenotypes of asthma and not all are mediated by allergies. Even so, we will first explore the allergy-driven TH2 hypothesis before describing some of the other theories of asthma pathogenesis.
What are the steps involved from being exposed to a piece of dust to developing wheezing? It is clear that this process does not happen to everyone and that only susceptible individuals have this problem. Over the last several decades there have been several basic immune mechanisms described including antibody-mediated and cell-mediated immunity, that are thought to be responsible for airways inflammation and obstruction in response to an allergic stimulus.
